News

Peripheral Arterial Disease – PAD
Peripheral artery disease (PAD) of the lower extremities is a common cause of impaired ambulation and is a leading cause of lower extremity wounds and amputations. It is also associated with atherosclerosis elsewhere in the body. Thus, individuals with PAD are at significantly increased risk of cardiovascular and cerebrovascular events and mortality.
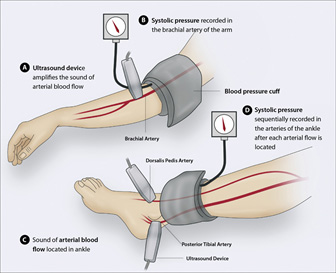
There is substantial evidence that the majority of cases of PAD go undetected in routine clinical practice. As a result, there is considerable interest in detection of PAD through routine screening. Whenever one suspects Peripheral Arterial Disease (PAD), the clinician must perform few non-invasive vascular testing methods that are commercially available and widely implemented. They include the ankle brachial index (ABI), the toe-brachial index(TBI), segmental Pressure Study and pulse volume recording(PVR).
Who is at risk for peripheral arterial disease?
The risk factors for getting peripheral arterial disease are similar to the risk factors for coronary heart disease, and include:
- Smoking cigarettes or using other forms of tobacco
- An abnormally high level of cholesterol
- An abnormally low level of high-density lipoprotein (HDL, the good cholesterol)
- High blood pressure (hypertension)
- Diabetes
- Family history of cardiovascular disease
- Obesity
- Physical inactivity (too little regular exercise)
- Kidney disease
What are the signs & Symptoms?
The most common symptom of peripheral arterial disease is intermittent claudication – pain or cramping in the legs or buttocks that starts when you exercise and goes away when you rest. Often the pain is described as a deep ache, especially in the calf muscle. The pain may extend to the foot or up toward the thigh and buttock. Sometimes, there is just numbness in the leg or a sense that one leg gets tired when you walk. A foot or toes also may feel cold or numb.
If the arteries are severely narrowed, you could experience leg pain at rest, when you are not exercising. If blood flow stops completely (usually because a blood clot forms in the narrowed vessel), parts of the leg may become pale or turn blue, feel stone cold to the touch and eventually develop gangrene.
Symptoms of poor kidney circulation include sudden high blood pressure, or blood pressure that is hard or impossible to control with medications. Severe blockage of the kidney arteries may result in loss of kidney function or failure.
Is peripheral artery disease dangerous?
Yes. In PAD, fatty deposits build up in the inner lining of artery walls. These blockages restrict blood flow, mainly in arteries leading to the kidneys, stomach, arms, legs and feet. Left untreated, PAD can lead to gangrene and amputation of limbs. If the blockage occurs in a carotid artery, it can cause a stroke. Most patients with PAD have a higher risk of death from heart attack and stroke. People with Diabetes having PAD have a very high risk of complications.
How is PAD diagnosed?
Diagnosing PAD begins with a medical history and physical exam.
To diagnose the PAD the following measurements are done
- Ankle Brachial Index (ABI)
- Toe Brachial Index (TBI)
- Pulse Volume Recording (PVR)
- Segmental Pressure
- Pulse Wave Velocity / Arterial Stiffness
- Vascular Age
- Percentage of Mean Arterial Pressure (MAP)
- Upstroke Time (UT)
TASC – II Guidelines:
| ABI Value | Interpretation | Recommendation |
|---|---|---|
| Greater than 1.4 | Calcification/Vessel Hardening | Refer to vascular specialist |
| 1.0 - 1.4 | Normal | None |
| 0.9 - 1.0 | Acceptable | None |
| 0.8 - 0.9 | Some Arterial Disease | Treat risk factors |
| 0.5 - 0.8 | Moderate Arterial Disease | Refer to vascular specialist |
| Less than 0.5 | Severe Arterial Disease | Refer to vascular specialist |
Toe-Brachial Index (TBI):
The digital arteries in great toes are considered to be less affected by medial arterial calcification. One would calculate TBI by dividing the blood pressure of the great toe by the systolic brachial blood pressure. Toe pressure of > 55mmHg is considered normal. Toe pressure < 30 mmHg is considered severely ischemic. Measurement of Toe systolic pressure drastically improves the reliability of distal blood pressure especially in diabetes. It is also useful for the diagnosis of critical limb ischemia and also assessment of healing potential of ulcers. TBI less than 0.7 is considered abnormal.
Low Toe-Brachial Pressure Index (TBI) Predicts Increased Risk of Recurrent Cardiovascular Disease in Type 2 Diabetes.
Segmental Limb Pressures:
Once the ABI has been performed, segmental limb pressure measurement can aid in localizing stenosis or occlusions. Limb pressure cuffs are placed on the thigh, below knee, ankle and digit. The pressure at each segment is measured. A difference in pressure of >30 mmHg between the cuff sites suggests a significant arterial stenosis or occlusion present between the site.
Pulse-Volume Recording:
Pulse-volume recordings (PVRs) are plethysmographic tracings that detect changes in the volume of blood flowing through a limb. Using equipment similar to the segmental limb pressure technique, pressure cuffs are inflated to 65 mm Hg, and a plethysmographic tracing is recorded at various levels. A normal PVR is similar to a normal arterial pulse wave tracing and consists of a rapid systolic upstroke and a rapid down stroke with a prominent dicrotic notch. With increasing severity of PAD, the waveforms become more attenuated with a wide down slope and, ultimately, virtually absent waveforms.
Arterial Stiffness and Cardiovascular Disease
There has been much recent interest in the relationship between arterial stiffness and cardiovascular disease. Surrogate measures of arterial stiffness indicate that arterial stiffness increases both with age and in certain disease states that are themselves associated with increased cardiovascular risk, including hypertension, diabetes mellitus, hypercholesterolemia and end-stage renal failure. As changes can be detected before the appearance of clinically apparent vascular disease, arterial stiffness may act either as a marker for the development of future atherosclerotic disease, or may be more directly involved of the process of atherosclerosis.
What is Pulse Wave Velocity?
Pulse Wave Velocity is the propagation speed of this wave along the arteries. Increased stiffness of the arteries increases Pulse Wave Velocity.
Age and systolic pressure strongly correlate with PWV. In fact, the most important factor contributing to increase in PWV is age because of increased arterial stiffness caused by medial calcification and loss of elasticity.
Heart rate is the frequency that the heart beats, and is an indicator of physical fitness. The more active you are, the lower your heart rate is. Blood pressure measures the pressure of blood on the arterial wall. It is one of the major cardiovascular risk factors, and can lead to an increased risk of stroke, heart failure, and kidney failure.
While heart rate and blood pressure measurements are useful in evaluating cardiovascular health, they do not give a complete picture of health. Pulse Wave Velocity, on the other hand, is an accurate stand-alone measurement of heart health.
What does the Pulse Wave Velocity say about my health?
Measuring Pulse Wave Velocity is recognized by the medical community as the best way to assess cardiovascular health, because it takes both arterial health and blood pressure variations into account.
“Decreasing PWV shows cardiovascular state improvement.” Professor Pierre Boutouyrie, European Society of Hypertension
“Elevated PWV is jointly associated with future systolic blood pressure and incident hypertention.” Dr. Gary Mitchell, Framingham Heart Study
Diseases such as diabetes, cholesterol or high blood pressure induce stiff arteries, which lead to an elevated Pulse Wave Velocity.
An elevated Pulse Wave Velocity is a sign of poor heart health, indicating a risk of having or developing high blood pressure. On the other hand, the more flexible the artery, the better your heart health.
What are the pathologic risks associated with high Pulse Wave Velocity?
Medical research has demonstrated a strong correlation between the stiffness of the arteries and the risk of a cardiovascular incident. Stiffer arteries indicate a greater risk for high blood pressure, stroke or heart attack.
Pulse Wave Velocity has been proven to be as reliable as the Framingham risk score, which is currently the most common way of predicting one’s risk of cardiovascular incident. Unlike the Framingham risk score, Pulse Wave Velocity is a direct measurement of your cardiovascular health.
Can I improve my Pulse Wave Velocity?
The good news is that you can decrease your Pulse Wave Velocity with healthy lifestyle changes. If you are overweight or obese, losing weight can have a tremendous impact. Engaging in physical exercise, and limiting salt and alcohol intake may also help to decrease your Pulse Wave Velocity. Additionally, managing stress can help you avoid elevated heart rate and blood pressure readings that can hurt your arteries over the long term.
What is vascular age?
The number of candles on your birthday cake may add up to your chronological age, but it doesn’t necessarily equal your biological age: environmental factors, such as stress and diet, and genetics can speed up or slow down how the body ages.
Vascular age is the apparent age of the blood vessels, particularly the arteries when compared to what is normal for the healthy population. Vascular age is affected by genetic predisposition, lifestyle choices and other factors.
Why is vascular age important?
A person whose vascular age is older than his or her chronological age may be at increased risk of developing cardiovascular disease later in life. The effects of early vascular aging may best be managed by early intervention.


